
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Head Neck Cancer Mucositis
Head Neck Cancer Mucositis
Head and neck cancer patients who undergo intensity-modulated radiation therapy (IMRT) are going to develop a side effect called mucositis or dry mouth. Well…not all patients but 98.6% of patients who undergo IMRT.
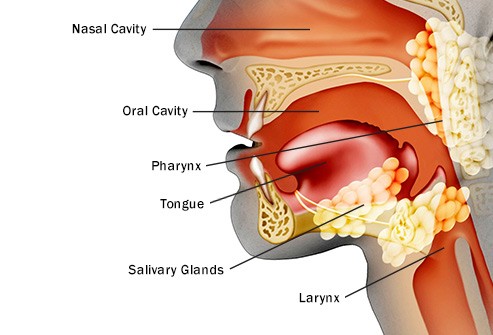
Mucositis is a common side effect of cancer treatment, particularly for patients undergoing radiation therapy and chemotherapy for head and neck cancer. It occurs due to damage to the mucous membranes lining the digestive tract, including the mouth, throat, and gastrointestinal tract. Here’s how it typically develops in head and neck cancer patients:
- Radiation Therapy: Radiation therapy is a common treatment for head and neck cancer. It uses high-energy rays to target and kill cancer cells. However, it can also damage nearby healthy cells, including the mucous membranes. The radiation disrupts the normal cell division process, leading to cell death and tissue damage.
- Chemotherapy: Some chemotherapy drugs used in head and neck cancer treatment can also cause mucositis. Chemotherapy affects rapidly dividing cells, which include both cancer cells and normal cells in the body. This includes the cells that line the mucous membranes.
- Direct Contact with Treatment Agents: During radiation therapy and chemotherapy, the treatment agents come into direct contact with the mucous membranes in the mouth and throat. This direct exposure can lead to irritation, inflammation, and damage to the mucosa.
- Inflammation and Ulceration: As a result of the damage, the mucous membranes become inflamed and may develop ulcers. These ulcers can be painful and make it difficult to eat, drink, and speak.
- Reduced Saliva Production: Radiation therapy, especially when directed towards the head and neck area, can also affect the salivary glands. This can lead to reduced saliva production, a condition known as xerostomia. Saliva plays a crucial role in protecting the oral mucosa, so its reduction can exacerbate mucositis.
- Compromised Immune System: Both radiation therapy and chemotherapy can weaken the immune system. This can make it harder for the body to repair damaged tissues and fight off infections, further contributing to the development and severity of mucositis.
- Secondary Infections: The damaged mucous membranes are more susceptible to bacterial, viral, and fungal infections. These secondary infections can worsen the mucositis and lead to additional complications.
As a cancer survivor who has struggled with this side effect since radiation to my neck in 1994, believe me that mucositis is a serious, painful side effect that can cause serious long-term damage to your health.
The bad news is that your oncologist may or may not prepare you for this side effects. The second study linked and excerpted below explains that conventional oncology’s mucositis treatment plan is to either give gabapentin ahead of time or wait for the patient to come to their oncologist once mucositis develops.
The good news is that there are several therapies shown to reduce and possibly heal mucositis.
I include myself in this group. I am not a head and neck cancer survivor but did undergo radiation to my lower neck (C5).
If you have been diagnosed with head and neck cancer and radiation is part of your treatment plan, consider evidence-based non-conventional therapies before, during and after IMRT therapy.
To learn more about evidence-based, non-conventional therapies for mucositis-
- Oral Mucositis- Prevent, Treat
- Pediatric Head & Neck Cancer- Mucositis
- Prevent Oral Mucositis in Nasopharyngeal Cancer
Have you been diagnosed with head and neck cancer? Have you already undergone radiation therapy and are experiencing dry mouth? Let me know- David.PeopleBeatingCancer@gmail.com
Thanks,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
High Rate of Severe Oral Mucositis After IMRT Seen in Head and Neck Cancer
“Many patients with head and neck cancer develop oral mucositis after intensity-modulated radiation therapy (IMRT), according to a single-center study published in JAMA Network Open.
The study also showed that most cases of oral mucositis were severe, and increasing severity of mucositis was associated with a greater likelihood of feeding tube placement, hospitalization, and opiate use…
The study included 576 patients who underwent definitive or adjuvant IMRT during 2015-2022…
Nearly all patients (98.6%) had oral mucositis, and 62.5% developed severe oral mucositis. By the final week of IMRT,
- 48.6% of patients had difficulty drinking,
- 56.8% had difficulty swallowing,
- and 69.4% had difficulty eating.
- Most patients (76.8%) were consuming a pureed diet and/or had a feeding tube by the end of IMRT…
Overall, 20.8% of patients required hospitalization. Hospitalizations occurred a median of 35 days from the start of IMRT, and the median length of stay was 4 days. The proportion of patients who required hospitalization was 25.0% in those who had severe mucositis and 13.9% in those who did not (P =.001).
The proportion of patients using opiates was 12.2% at the start of IMRT and 50.9% by the end of treatment. The proportion of patients using opiates was 63% among those who had severe mucositis and 35% among those who did not (P <.001).
“These findings suggest that oral mucositis continues to cause morbidity in patients with head and neck cancer, contributing to worse quality of life and financial effects,” the researchers concluded.”
Severe Oral Mucositis After Intensity-Modulated Radiation Therapy for Head and Neck Cancer
“Management of OM varies greatly at different institutions. Our institutional standard strongly emphasizes oral hygiene, hydration, and nutrition at the start of treatment and uses prescription medications when necessary as patients develop worsening OM symptoms.16
For OM pain control, we prescribe all eligible patients prophylactic gabapentin and recommend alternating between over-the-counter acetaminophen and nonsteroidal anti-inflammatory drugs before prescribing opioids. The use of prophylactic gabapentin is controversial, with multiple studies34–38 showing it can reduce and delay opioid use in patients with HNC, while a placebo-controlled randomized clinical trial39found it to have no pain control benefit.
Consistent with prior reports,4–6 we found severity of OM to be associated with opiate use. Patient pain control continues to worsen during treatment despite opioid prescriptions, indicating better solutions are still desperately needed…”

