Seve Tierra was diagnosed with Light Chain Deposition Disease (LCDD) in 2015. Seve’s kidney function was severely impaired and had microscopic blood in his urine. But Seve also had indicators of a blood cancer called multiple myeloma in his bone marrow.
Multiple Myeloma Stages
Both LCDD and multiple myeloma are rare diseases. According to the article linked below, LCDD is found in 5% of myeloma patients upon autopsy. Myeloma is a rare blood cancer comprising 1.8% of all cancer diagnoses in the U.S. annually and 10% of all blood cancer cases in the U.S. annually.
The question then, is if LCDD is a symptom of multiple myeloma, or is LCDD a disease all by itself?
Interestingly enough, though LCDD is “associated with multiple myeloma,” and it may progress to multiple myeloma eventually, according to the top article linked below, LCDD is not a symptom of multiple myeloma. It is a separate disease.
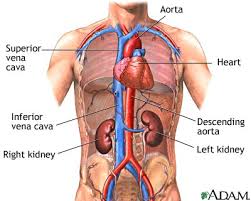
The common denominator in studying both MM and LCDD is light chains and kidney function. And if the patient has impaired kidney function, the real issue is how to treat the kidney in order to make it function properly again.
Light Chain Deposition Disease
Light chains can gum up your heart, lungs, and kidneys of course. But the presence of light chains, by itself, doesn’t always mean you have multiple myeloma.
Myeloma making light chains which then damage the patient’s kidney function is common enough. According to research, between 20% and 40% of NDMM patients present with kidney involvement when they are first diagnosed.
In my experience then, the challenge is two-fold in myeloma patients with kidney disease.
- First, the patient must treat his/her myeloma. After all, it’s the myeloma that is making the light chains to begin with.
- Secondly, the patient must treat his/her kidney damage. Because myeloma is an incurable blood cancer, any myeloma growing in the patient’s bone marrow can make light chains which will in turn damage the kidneys.
And here is the kicker. Many chemo regimens can cause kidney damage. Bisphosphonates, bone strengthening therapy, can also cause kidney damage.
Here’s how Seve’s oncologist managed his myeloma and by extension his Light Chain Deposition Disease. In short, low dose chemotherapy. To be more specific:
- Bortezomib (Velcade)
- Cyclophosphomide (Cytoxan)
- Dexamethasone
Long story short, Seve’s low-dose chemotherapy regimens since his diagnosis in 2015 has stabilized his
- kidney function
- monoclonal proteins
- freelight chains
- bone health etc.
All as measured by diagnostic testing. In effect, Seve and his doctors treated two rare diseases, light chain deposition disease and multiple myeloma, managing to put Seve in complete remission from each.
Light chains are an important issue in the treatment of multiple myeloma-
Have you been diagnosed with Light Chain Deposition Disease? Scroll down the page, post a question or comment and I will reply to you ASAP.
To learn more about kidney involvement in pre-myeloma stages- click now
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
The underlying cause of LCDD is unknown. It is often associated with multiple myeloma. LCDD may progress to multiple myeloma, or it may be present with multiple myeloma when it is first diagnosed.
The goal of treating LCDD is to slow the production of light chains and their damage to organs. Treatment may include chemotherapy with a drug called Bortezomib; autologous stem cell transplantation; immunomodulatory drugs; and/or kidney transplant. If untreated, end-stage renal disease occurs in 70% of cases.[2204][11958][11959]
“Light-chain deposition disease (LCDD) is the deposition of monoclonal light chains in multiple organs. It is a rare disease characterized by deposition of nonamyloid immunoglobulin light chains, which unlike amyloid do not stain with Congo red and do not exhibit a fibrillar structure when examined ultrastructurally. [1, 2, 3, 4]…
A single clonal plasma cell is responsible for the overproduction of kappa chains and more rarely, lambda light chains. [8] These light chains may be in association with a heavy chain as a complete antibody or be secreted as only a collection of light chains or as a combination of both, [9] although in LCDD only light chains will be observed.
A monoclonal population of plasma cells can be detected in the bone marrow, and an altered serum-free light chain ratio is present. [10]
In 25% of patients, an abnormal serum free light chain ratio is noted, even without an abnormal finding with serum and/or urine electrophoresis with immunofixation. [11]…
LCDD can occur in any organ. [12] Kidneys are nearly always involved, and LCDD can present as
kidney insufficiency,
proteinuria,
microscopic hematuria, and
nephrotic syndrome…
The approach for diagnosis with LCDD should be the same as for patients with plasma cell dyscrasias. [18] It should include a thorough history, physical examination, and laboratory and imaging studies.
LCDD should be distinguished from:
- Fanconi syndrome,
- myeloma cast nephropathy,
- cryoglobulinemia, and
- amyloidosis,
all of which are also associated with monoclonal proteins and may present similarly…
LCDD is a rare disease, so no established guidelines exist and management remains controversial. [19] Treatment options include the following:
Amyloid light-chain (AL)–amyloidosis consists predominantly of lambda light chains, whereas kappa light chains are predominantly involved in LCDD. Electron microscopy is helpful in distinguishing between these lesions…
LCDD is associated with multiple myeloma is about 58% of cases. [5] LCDD could be present at diagnosis of a new plasma cell dyscrasia or could represent an extramedullary manifestation of multiple myeloma while relapsing after chemotherapy. [29]…
The frequency of light-chain deposition disease (LCDD) is unknown. The disease is found in approximately 5% of patients with multiple myeloma at autopsy…
“Kidney failure and damage are common complications of multiple myeloma, a type of blood cancer. But there are several treatment options to help counteract kidney failure…
Multiple myeloma’s effect on the kidneys
Kidney failure in multiple myeloma is a complicated process that involves various mechanisms. The primary cause of this kidney failure is abnormal proteins called monoclonal light chains.
Multiple myeloma cells make monoclonal light chains, which travel to the kidneys and deposit themselves there.
Monoclonal light chains can have a toxic effect on the kidneys’ tubules and glomeruli. Tubules are small tubes that help filter waste. Glomeruli are capillaries, or small blood vessels, located on the ends of tubules.
Monoclonal light chains can obstruct the tubules and alter the kidneys’ filtering properties…