Leave a Comment:
2 comments
I don’t feel as dumb now, thank you. I can’t mention this in the support group….would not go well.
Thank you, David

Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
While a hematopoietic stem cell transplant, according to the first two studies linked below, potentially curative for many patients, ASCT is NOT curative for multiple myeloma patients. In fact, bone loss is one of many different side effects that can result from a stem cell transplant.
I am okay with the patient choosing to pursue risky procedures if their disease gives them little or no choice. But this is not the case with newly diagnosed patients with my cancer- multiple myeloma. MM patients have a choice.
It’s important that I stress that chemotherapy and radiation both have risks in the treatment of cancers. I don’t dispute this. I’m saying that hematopoietic stem cell transplantation is aggressive, high dose chemo that is a choice for the multiple myeloma patient. Many studies question the benefit of ASCT over novel chemotherapy regimens for the long-term treatment of MM.
Ask your oncologist what, if any, additional length of life an ASCT is supposed to give MM patients. If he/she is honest with you, the answer is none. On average, no additional OS for those MM patients who undergo an ASCT.
I think that being an oncologist is a difficult job. Multiple myeloma is a rare cancer encompassing less that 2 percent of the annual cancer diagnoses in the United States annually. The majority of oncologists have little if any experience with this incurable blood cancer.
I can’t blame general oncologists and hematologists for not understanding the many long-term side effects of hematopoietic stem cell transplantation. Especially since the FDA approved standard-of-care for the treatment of newly diagnosed myeloma patients include hematopoietic stem cell transplantation.
Are you a newly diagnosed myeloma patient? Please don’t expect your oncologist to thoroughly explain the short, long-term and late stage side effects that can result from this aggressive procedure.
To learn more about MM, scroll down the page, post a question or a comment and I will reply to you ASAP.
Hang in there,
David Emerson
“Hematopoietic stem cell transplantation (HSCT), including bone marrow transplantation, is the treatment of choice for many hematologic diseases, including hematologic malignancies and different types of anemia.
The use of HSCT is increasing annually, mainly because advanced research that has been conducted in this area has exponentially expanded the indications for HSCT and significantly improved transplantation techniques and supportive care practices.
Collectively, these improvements have led to an increase in the overall survival of HSCT patients. However, as post-HSCT survival is increasing, awareness of the potential late complications of HSCT is also growing.
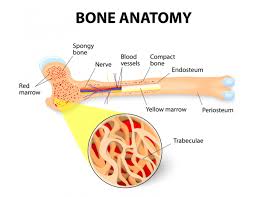
Unpredictable bone loss is one of the major post-HSCT complications that can cause significant morbidity and impair the quality of life of survivors.
Although the exact mechanism of post-HSCT bone loss is not yet known, previous studies have suggested that numerous factors, including
are responsible for HSCT-associated bone loss. Sufficient data have been collected to suggest that post-HSCT bone loss can be prevented and treated using the same preventive and treatment modalities as used for the general population. Various guidelines have been formulated to help keep a check on HSCT recipients’ deteriorating bone health.
“Autologous and allogeneic hematopoietic stem cell transplantation (HSCT) is the treatment of choice for patients with some malignant and non-malignant hematological diseases. Advances in transplantation techniques and supportive care measures have substantially increased the number of long-term HSCT survivors.
This has led to an increasing patient population suffering from the late effects of HSCT, of which, bone loss and its consequent fragility fractures lead to substantial morbidity.
Altered bone health, with consequent fragility fractures, and chronic graft-versus-host disease (GVHD) are factors affecting long-term quality of life after HSCT. Hypogonadism, HSCT preparative regimens, nutritional factors, and glucocorticoids all contribute to accelerated bone loss and increased fracture risk.
Management strategies should include bone mineral density examination, evaluation of clinical risk factors, and general dietary and physical activity measures. Evidence has accumulated permitting recommendations for more attentiveness to evaluation and monitoring of bone health, with appropriate application of osteoporosis pharmacotherapies to patients at increased risk of bone loss and fracture.
“Annually, ~50,000 patients undergo hematopoietic stem cell transplantation (HCT) worldwide with almost 22,000 of these patients receiving HCT in the United States…
It is anticipated that the number of HCT survivors will more than double from 242,000 in 2020 to ~500,000 in 2030. Survivors of HCT are at an increased risk of developing late complications due to exposure to chemotherapy and/or radiation in the pre-, peri-, and post-HCT phases and these cumulative exposures have the potential to damage normal tissue.
This tissue damage leads to the early onset of chronic health conditions resulting in premature mortality in HCT survivors, who have a 15-year cumulative incidence of severe or life-threatening chronic health conditions exceeding 40%.
Due to the significant burden of morbidity in HCT survivors and the delay in the development of long-term complications, this delicate patient population requires life-long monitoring due to the risk for neuropsychological, cardiac, pulmonary, renal, hepatic, ocular, skeletal, cardiac, endocrine, fertility, and sexual health complications, as well as secondary neoplasms…”
I don’t feel as dumb now, thank you. I can’t mention this in the support group….would not go well.
Thank you, David