
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- non-conventional therapies »
- Radiation-induced Spindle Cell Sarcoma
Radiation-induced Spindle Cell Sarcoma
From: Jane
Subject: Sarcoma
Dear David:
12 years ago breast cancer operated on, Radiation and chemo. 3 years ago a spindle cell sarcoma operated on with radiation . Today sarcoma has returned. Diagnosis: Chemo, radiation, operation
Hi Jane-
I am sorry to learn of your spindle cell carcinoma relapse. For the sake of this email I am going to assume that your BC is, and will continue to remain in complete remission.
Though you don’t ask any questions in your email I am going to assume that you are wondering about your prognosis and therapy recommendations (chemo, radiation, operation). Further, I will assume that your original diagnosis of spindle cell carcinoma was early stage and that a relapse means that the cancer has metastasized.
To be able to research and relay issues such as evidence-based therapies, (both potentially curative and palliative) as well as possible side effects I need to know the stage of your cancer currently, where the cancer has metastasized, and what, if any, symptoms you are currently experiencing.
The study linked and excerpted below talks about the importance of genetic expression of spindle cell sarcoma when determining your prognosis.
Let me know, thanks.
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
“These results suggest that the combination analysis of p27(Kip1) and cyclin E expression even in biopsy specimens allows the prediction of the clinical behavior of spindle-cell sarcoma.”
Thanks David,
I don’t know the stage? We are going on the 12th to find out more. It seems that the sarcoma is growing out not inside. I know you can’t answer questions without more info. We hate Chemo and will try not to get any more. Here is an image of the sarcoma. Thanks
Jane-
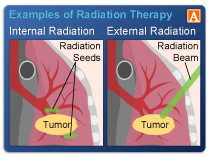
The photo implies that the local radiation for Jane’s BC caused the sarcoma. Interestingly,
“The average time between the radiation treatments and the diagnosis of a sarcoma is about 10 years.”
The pubmed article linked below will focus the issues for your next appointment. I am not an onc. nor am I an expert in the field of radiation-induced sarcoma. However it is clear to me that Jean’s cancer diagnosis is rare and complicated.
I think you and Jean should pursue a multi-modal approach to her cancer therapy meaning every evidence-based therapy from conventional to integrative, complementary, nutritional, mind-body and lifestyle therapies. Your onc. should be able to address conventional therapies while I can address all non-conventional therapies.
Let me know if you have any questions.
thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Radiation-induced sarcoma.
“Radiation-induced sarcomas can originate in either the irradiated bone or soft tissues. Most of these tumors are high-grade. The most common histologic subtypes are malignant fibrous histiocytoma (MFH) and osteosarcoma, although other histologies (eg, angiosarcoma, rhabdomyosarcoma) can occur.
Tumor size and grade are the two most important prognostic factors for soft tissue sarcomas, including those associated with radiation therapy. The therapy is therefore dictated by the risk of distant metastases.
High-grade tumors that are larger than 5 cm should be treated with primary chemotherapy followed by a margin-negative surgical excision of the residual disease. All low-grade tumors and high-grade tumors 5 cm or smaller should be treated with a margin-negative surgical excision, and systemic chemotherapy should be considered when a negative margin is difficult or impossible to accomplish.
Radiation-induced sarcomas (either MFH or osteosarcoma) originating in bone should be approached with primary chemotherapy followed by a margin-negative excision similar to de novo bone sarcomas. The dose-intensity of the active agents should be adjusted appropriately for the age, performance status, and prior therapy in a given patient.”

