
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Radiation-induced- Dermatitis, Dysphagia, CIPN, RILP
Radiation-induced- Dermatitis, Dysphagia, CIPN, RILP
I’ve written about my cancer, multiple myeloma, since launching PeopleBeatingCancer.org in June of 1994. I began to research and write about my more obvious long-term and late stage side-effects such as chemotherapy-induced brain and heart damage about 10 years later. Coming across the article linked and excerpted below got me thinking about pain. Radiation-induced pain to be specific.
My first course of radiation therapy was to my fifth cervical vertebra. I had just had a single plasmacytoma removed from the area and my oncologist called for local radiation to sort of clean-up the area- make sure there were no stray multiple myeloma (MM) cells in the area.
This use of local radiation was ineffective. I was diagnosed with full multiple myeloma less than a year later.
The second and third courses of local radiation were to my iliac crest. Imaging indicated that MM lesions were growing in and around my sacrum. Local radiation was considered to be palliative therapy.
Both courses of radiation eliminated the lesions, stopped the nerve and bone pain- at least for a few months. And, as strange as this may sound, this palliative therapy gave me the time I needed to find the therapy (Antineoplaston therapy- ANP) that put me into complete remission in early 1999. Where I remain today.
The purpose of this post then, is to document radiation-induced pain.
The article linked below talks about those specific types of pain caused by radiation therapy. I have excerpted the original article to cover only those types of radiation-induced pain that I live with. Specifically:
- radiation dermatitis,
- radiation fibrosis,
- dysphagia
- radiation-induced lumbosacral plexopathy
- chemotherapy-induced peripheral neuropathy
I can’t say that I’ve figured out how to eliminate all of my radiation-induced pain. But I have figure out many coping methods that reduce my pain and turn it into manageable pain.
If you recognize any of the examples discussed below and you would like to learn about my therapies to manage this pain, scroll down the page, post a question or comment and I will reply to you ASAP.
- To Learn More about Chronic Non-Cancer Pain- click now
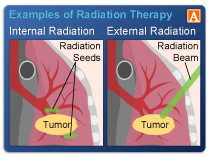
- To Learn More About the pros and cons of Ionising Radiation- click now
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Side Effects- Radiation-Induced Lumbosacral Plexopathy
- End Stage Multiple Myeloma- Early Palliative Care
- Velcade/Bortezomib- CIPN, Heart, Blood, Muscle Damage
Review: Pain of Radiation Therapy Increases With Frequency of Its Use
“As the understanding of cancer therapies has evolved, the use of radiation therapy has increased. The treatment paradigm for solid cancers increasingly relies on radiation therapies, but currently the chronic effects associated with these treatments are poorly characterized. In fact, the use of radiation therapy has increased significantly in the past 2 decades — meaning that the recognition and understanding of radiation-specific chronic pain is now critical…
Burden of Chronic Pain
“Post-treatment chronic pain syndromes in patients with cancer are associated with a plethora of quality of life detriments, including psychological distress, immobility, and even disability,” the review authors wrote. “These pain syndromes can also manifest during cancer treatment and affect ongoing treatment candidacy…
Incidence Outpaces Information
According to the review authors, an increase in cancer survivorship is at least partially responsible for the increase in chronic pain prevalence among people with cancer. Tumor type, tumor severity, and cancer treatment strategies all factor into the pathogenesis of chronic pain, with estimates indicating chronic pain in 50% of those with early cancer and 75% of those with advanced disease….
Classification Challenges
The study authors point out that the multiple challenges in classifying radiation therapy-associated pain syndromes include the heterogeneous nature of the conditions, when the patient presents with the condition, and the concomitant use of chemotherapies and surgical procedures in these patients. Radiation-specific pain syndromes can manifest in a various organ systems and can become apparent either early or late in the treatment course.
Specific chronic pain patterns manifest in certain cancers. For example, people with breast cancer — the cancer with the highest number of survivors who have undergone radiation therapy — are vulnerable to conditions like brachial plexopathy or upper extremity lymphedema. In contrast, people with gynecologic cancers are more likely to develop radiation enteritis.
Understanding Radiation Therapy Toxicity
Damage to DNA is the driving mechanism behind the biological effects of radiation therapy. Radiation therapy-induced inflammatory cytokines, then, are responsible for the acute systemic effects…
It is critical to consider clinical and temporal factors when determining radiation therapy-related toxicity. When determining the probability of late radiation effects, important factors include the radiation therapy dose, tissue type targeted, tissue volume irradiated, and the time since treatment…
Overview of Radiation Therapy-Specific Pain Syndromes
The following 7 pain syndromes must be given individual examination: dermatitis, oral mucositis, acute radiation enteritis, chronic abdominal pain, local connective tissue fibrosis, lymphedema, and neuropathic pain syndromes.
Dermatitis
Posttreatment dermatitis occurs in roughly 95% of people who undergo radiation therapy. Early symptoms include erythema, pigment color changes, edema, depilation, and radiation burns. While most symptoms typically occur within 90 days of treatment, transient erythema can occur as soon as 2 hours posttherapy.
Chronic radiation dermatitis symptoms include scaly skin, hyperkeratosis, pigment changes, telangiectasia, alopecia, nail changes, slow-healing erosions or ulcers, and soft tissue, bone, and cartilage necrosis, among others. Patients with head and neck cancers or breast cancers are most susceptible to the late complications of primary dermatitis, according to the review authors, due to the radiation-specific skin sensitivity of the face, neck, and chest. Because the mechanism of radiation therapy induces DNA damage, and cutaneous tissue and skin cells are among “the most regenerative,” these areas are highly vulnerable to experiencing radiation injury.
Prevention and treatment options are varied. Superficially, proton therapy can more accurately direct high-dose radiation therapy to target structures, sparing the critical structures below. Other prevention options include good skin hygiene, moisturizers, and decreased sun exposure. But, the review authors caution, emollients must be compatible with radiation therapy, and should not be applied in the hours before treatment.
Acute radiation dermatitis severity is graded on a 1-to-4 scale by the National Cancer Institute. 3 Grade 1 is described as faint erythema, while grade 4 is described as skin necrosis or ulceration and may include spontaneous bleeding in the affected area.
Treatments, then, vary based on dermatitis grade: for grades 2 and 3, hydrocolloid and hydrogel dressings can be used, while for grade 4, lesions may require surgical debridement with skin flaps. Evidence for the use of vitamins C and E and beta-carotene antioxidants is limited. Studies have reported supportive evidence for the use of pentoxifylline which, in combination with vitamin E, may increase tissue vascularity.3,4
For radiation-induced cutaneous fibrosis, deep-friction massage, therapy, and orthotics have been proposed as possible treatments.5,6 Gabapentin, pregabalin, duloxetine, and tricyclic antidepressants may be used in conjunction with nonsteroidal anti-inflammatory drugs (NSAIDs) for nociceptive and neuropathic pain.6,7…
Connective Tissue Fibrosis
Local connective tissue fibrosis is assumed to underlie the late effects of radiation therapy, but the pathophysiology is uncertain. Three phases are suggested for radiation-induced fibrosis: endothelial cell dysfunction associated with chronic, nonspecific inflammation at the radiation site, fibroblast activation to secrete disorganized extracellular matrix, and further remodeling of the extracellular matrix leading to dense sclerotic tissue and poor vascularization.
Many patients who have radiation fibrosis syndrome experience debilitating chronic pain. Clinical presentations vary depending on which anatomic structures radiation therapy targets as well as on the use of concomitant treatments such as surgery or chemotherapy.
Any person who receives radiation therapy at any site that contains “critical neuromuscular structures” can be at risk for radiation fibrosis syndrome. Patients with head and neck cancers are among the most at risk, with from 20% to 60% of these patients experiencing radiation fibrosis syndrome, while 30% of breast cancer patients experience it. Complications such as radiculopathy and plexopathy may occur and manifest as weakness or sensory changes in the nerves. Myopathy due to muscle fiber fibrosis may cause contractures in head, neck, and shoulder girdle muscles.
The primary treatment for radiation fibrosis syndrome is comprehensive physical and rehabilitative therapy. Neuromuscular re-education can correct movement and postural problems, and myofascial release has improved pain, range of motion, and motor functionality. Medications such as pregabalin, gabapentin, duloxetine, and tricyclic antidepressants can be used to manage both neuropathic and muscular pain, while opioids can be “cautiously considered” if appropriate. Combination pentoxifylline and vitamin E is hypothesized to have anticytokine activity, and some evidence suggests this combination is helpful as both a preventive and therapeutic measure.17,18…
Neuropathic Pain Syndromes
Radiation therapy is associated with a host of neurotoxic adverse effects and radiation-specific peripheral neuropathies, resulting in gradual and irreparable nerve damage over the course of several years. Pathophysiology of these processes is not fully understood, but 3 key factors have been identified: indirect compressional damage from radiation-induced fibrosis, direct axonal damage and demyelination, and neural ischemia from microvascular injury.
Radiation-induced brachial plexopathy is, according to the review authors, one of the most feared complications. The condition typically results in mild paresthesia, numbness, swelling, weakness, and debilitating pain in distal upper extremities. These symptoms can, in some patients with severe presentations, progress to paralysis. Pain occurs in half of all patients but is generally mild to moderate. Severe pain is representative of new or increased tumor burden.
Radiation-induced lumbosacral plexopathy is another debilitating condition, often occurring after pelvic, colon, and testicular cancers or para-aortic lymph node tumors. Onset is typically within 1 year of treatment but can be delayed up to 31 years. Disease progression is slow and classified by sensory changes, muscle atrophy, fasciculations, and abnormal deep tendon reflexes. Pain is an uncommon presenting symptom.
For both conditions, radiographic imaging is required to rule out tumor-based etiology. However, treatment options are mostly symptomatic, and the goal is managing pain and improving function and quality of life. Prevention strategies include using the minimum effective radiation dose.
For radiation-specific peripheral neuropathies secondary to radiation-induced fibrosis, early physical therapy can slow progression of muscular atrophy and sensory and motor defects. Medication management includes corticosteroids, anti-inflammatory agents, pentoxifylline, and hyperbaric oxygen vascular therapy. Studies, though, are inconsistent and suggest an “unpredictable patient response.” Neurolysis with omentoplasty for revascularization provides short-term pain relief, but long-term prognosis is unclear.22,23
Pregabalin and botulinum neurotoxins improve pain, mood, and quality of life in symptomatic treatment for both radiation-induced peripheral neuropathy and postsurgical pain. Evidence suggests that botulinum neurotoxins have direct analgesic properties, decreasing the release of noxious neurotransmitters including substance P and calcitonin gene-related peptide.23,24 Other medication options include nonopioid analgesics, muscle relaxants, benzodiazepines, tricyclic antidepressants, and antiepileptics.
Delayed-onset radiation-induced myelopathy is observed in patients who receive radiation therapy in the cervical and upper thoracic region. Pathogenesis is hypothesized to stem from glial cell and microvascular damage; glial cells are stimulated by direct radiation damage to produce vascular endothelial growth factor, leading to increased vascular permeability, edema, and damage. Radiation-induced myelopathy typically occurs around 6 months after radiation therapy but can present up to 10 years afterwards; 75% of patients present with symptoms within 2.5 years…
“Understanding these unique pain syndromes is paramount, given that the diagnosis and management of these conditions can serve to present long-standing functional impairments, optimize quality of life, and even allow for continued [radiation therapy] candidacy,” the researchers concluded. “It is necessary to maintain a low threshold of suspicion for appropriately diagnosing these conditions, as there exists a variance in when these symptoms arise after radiation.”
Disclosure: Some review authors declared affiliations with the pharmaceutical industry. Please see the original reference for a full list of authors’ disclosures.


