Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Axillary Node Dissection in DCIS Offers Little Prognostic Information
Axillary Node Dissection in DCIS Offers Little Prognostic Information

“If it’s pure DCIS, don’t do the sentinel biopsy, because you have less than a 1% chance of it being positive and greater risks of developing other complications.”…
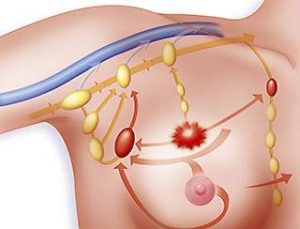
I was stunned when I first found out that lymph nodes were being sampled for those with many forms of DCIS. The axillary node dissection which was used in the earlier years of this study has a high potential for causing lymphedema. The sentinel node biopsy that is often currently performed has a lower chance of causing lymphedema, but it is not a negligible chance. It is well worth the risk if you have invasive breast cancer, but, in my opinion, would almost never be worth the risk in pure DCIS.
Another recent article “Ductal carcinoma in situ of the breast: a systematic review of incidence, treatment, and outcomes” which is included on People Beating Cancer reaches a slightly different conclusion.
“A new study presented at the American Society of Breast Surgeons (ASBrS) 11th Annual Meeting indicates that 2 commonly used procedures — axillary node dissection and sentinel lymph node biopsy — might pose more harm than good to patients with pure ductal carcinoma in situ (DCIS).
Amy Bremner, MD, a surgeon at Hoag Memorial Hospital Presbyterian in Newport Beach, California, told Medscape Oncology that her findings indicate that not only do these procedures and their subsequent findings not affect survival “in any way,” the procedure itself carries some morbidity — albeit low. “So unless there are circumstances that have an invasive component,” she said, “we would say do not do it.”
For more information about breast cancer therapies- conventional, integrative or alternative, scroll down the page, post a question or comment and I will reply ASAP.
To learn more about DCIS and the evidence-based therapies that can help you prevent its spread into invasive breast cancer, please watch the video below:
Mary Miller-BC Profile in Courage
Axillary Node Dissection in DCIS Offers Little Prognostic Information
“A new study presented here at the American Society of Breast Surgeons (ASBrS) 11th Annual Meeting indicates that 2 commonly used procedures — axillary node dissection and sentinel lymph node biopsy — might pose more harm than good to patients with pure ductal carcinoma in situ (DCIS)…
Other adverse effects that can accompany sentinel node biopsy are arm pain and inflammation. “What you want to do is minimize the risk and minimize the morbidity,” said Dr. Attai. “If it’s pure DCIS, don’t do the sentinel biopsy, because you have less than a 1% chance of it being positive and greater risks of developing other complications.”…
Sentinel lymph node biopsy can be omitted in DCIS patients treated with breast conserving therapy
“Breast cancer guidelines advise sentinel lymph node biopsy (SLNB) in patients with ductal carcinoma in situ (DCIS) on core biopsy at high risk of invasive cancer or in case of mastectomy. This study investigates the incidence of SLNB and SLN metastases and the relevance of indications in guidelines and literature to perform SLNB in order to validate whether SLNB is justified in patients with DCIS on core biopsy in current era.
Clinically node negative patients diagnosed from 2004 to 2013 with only DCIS on core needle biopsy were selected from a national database. Incidence of SLN biopsy and metastases was calculated. With Fisher exact tests correlation between SLNB indications and actual presence of SLN metastases was studied.
Further, underestimation rate for invasive cancer and correlation with SLN metastases was analysed. 910 patients were included. SLNB was performed in 471 patients (51.8 %): 94.5 % had pN0, 3.0 % pN1mi and 2.5 % pN1. Patients undergoing mastectomy had 7 % SLN metastases versus 3.5 % for breast conserving surgery (BCS) (p = 0.107).
The only factors correlating to SLN metastases were smaller core needle size (p = 0.01) and invasive cancer (p < 0.001). Invasive cancer was detected in 16.7 % by histopathology with 15.6 % SLN metastases versus only 2 % in pure DCIS. SLNB showed metastases in 5.5 % of patients; 3.5 % in case of BCS (any histopathology) and 2 % when pure DCIS was found at definitive histopathology (BCS and mastectomy). Consequently, SLNB should no longer be performed in patients diagnosed with DCIS on core biopsy undergoing BCS. If definitive histopathology shows invasive cancer, SLNB can still be considered after initial surgery…”