“…our findings offer strong support for the view that in some individuals, monoclonal gammopathy has the potential to cause systemic disease resulting in wide-ranging organ/tissue damage and excess mortality.”
Yes, MGUS can kill you. But so can obesity, so can the flu and so can a bunch of other health problems. I’m trying to make two points. First, the chances of dying from MGUS is very low. Secondly, you can dramatically lower your odds of dying from MGUS, the flu or from obesity by taking relatively simple steps.
Or to flip this idea, you don’t need to take dramatic steps to reduce your risk of pre-myeloma (SBP, MGUS or SMM). You don’t need to take dramatic steps to reduce your risk of dying from the flu or from obesity either. I’ll stick with MGUS because this is a blog post about pre-myeloma.
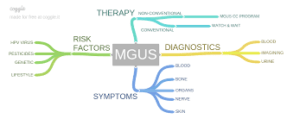
Before I talk about reducing your risk of problems due to MGUS symptoms, I need to clarify why an “asymptomatic” form of pre-myeloma can cause symptoms.
Monoclonal gammopathy of undetermined significance increases the risk of the symptoms listed below. It is these symptoms than can increase the risk of death for the MGUS patient.
I’ll tell you what happened to me to explain what I mean. In the fall of 1993, I developed a pain in my neck. For a couple of months I ignored this pain. The pain was minimal at first and I didn’t want to make an appointment with my doctor simply because I had a pain in my neck…
Eventually the pain because severe enough that I went to one of those emergency clinics on the way home from work one day. The doctor on duty took an x-ray of my neck, identified a mass where my fifth cervical vertebra was supposed to be. I went to the hospital ASAP.
Long story short, asymptomatic pre-myeloma eventually became symptomatic. The monoclonal proteins (MM cells) growing in my C5 grew/multiplied and caused my C4 vertebra to collapse onto my c6 vertebra. I developed several of the symptoms listed below- pain, nerve pain and bone pain-
It was my symptomatic pre-myeloma that increased my risk of death. I distinctly remember the doctor looking at the x-ray with an unidentified mass where my C5 was supposed to be and told me that getting into a car accident might cause my neck to break.
My asymptomatic pre-myeloma became symptomatic pre-myeloma. I still hadn’t reached full-blown multiple myeloma but I had developed symptoms and I was close to how the study linked below explains MGUS and the risk of death- “our findings offer strong support for the view that in some individuals, monoclonal gammopathy has the potential to cause systemic disease resulting in wide-ranging organ/tissue damage and excess mortality.”
The point of all this is simply that MGUS increasing the risk of death isn’t as far-fetched as it sounds.
Further, evidence-based, non-toxic, non-conventional therapies such as anti-angiogenic nutrition, anti-angiogenic supplementation and a number of lifestyle therapies such as frequent, moderate exercise have been shown to reduce the risk of multiple myeloma.
Nutrition and supplementation (zinc, vitamin C, omega-3, vitamin D3, others) have been shown to reduce your risk of influenza as well as the coronavirus.
To learn more about evidence-based, non-conventional therapies scroll down the page, post a question or comment and I will reply to you ASAP.
Thanks very much for your time and attention,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
OBJECTIVE: To examine mortality and morbidity patterns before and after premalignancy diagnosis in individuals with monoclonal gammopathy of undetermined significance (MGUS) and monoclonal B-cell lymphocytosis (MBL) and compare their secondary healthcare activity to that of the general population…
MAIN OUTCOME MEASURES: Mortality and hospital inpatient and outpatient activity in the 5 years before and 3 years after diagnosis.
RESULTS: Individuals with MGUS experienced excess morbidity in the 5 years before diagnosis and excess mortality and morbidity in the 3 years after diagnosis. Increased rate ratios (RRs) were evident for nearly all clinical specialties, the largest, both before and after diagnosis, being for nephrology (before RR=4.29, 95% CI 3.90 to 4.71; after RR=13.8, 95% CI 12.8 to 15.0) and rheumatology (before RR=3.40, 95% CI 3.18 to 3.63; after RR=5.44, 95% CI 5.08 to 5.83). Strong effects were also evident for endocrinology, neurology, dermatology and respiratory medicine. Conversely, only marginal increases in mortality and morbidity were evident for MBL.
CONCLUSIONS: MGUS and MBL are generally considered to be relatively benign, since most individuals with monoclonal immunoglobulins never develop a B-cell malignancy or any other monoclonal protein-related organ/tissue-related disorder.
Nonetheless, our findings offer strong support for the view that in some individuals, monoclonal gammopathy has the potential to cause systemic disease resulting in wide-ranging organ/tissue damage and excess mortality.”