Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Myeloma Q & A- Bone Involvement
Myeloma Q & A- Bone Involvement
Should we treat patients with myeloma with multidrug, multitransplant combinations with the goal of potentially curing a subset of patients, recognizing that the risk of adverse events and effect on quality of life will be substantial?
Hi, I’m a Multiple Myeloma patient 4 years into it. The cancer is under control with Darzelex and polmalyst. I’m very concerned about my bone health. I have many lesions along my spine, ribs with a 2cm in the sacral area. I was treated with Zometa early on but developed necrosis of the jaw (ONJ).
Do you have any recommendations for keeping my bones healthy? Currently I have no fractures but worried about the future as I am an active person. I am taking vitamin D 3000mg , turmeric and CBD. Fred
Hi Fred,
Good to read that you are managing your MM. Four years is a good start.
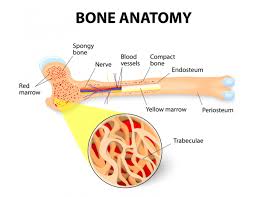
In my experience, MM is as much of a bone disease as it is a bone marrow disease. I too had lots of lesions, lots of bone damage. While bisphosphonate therapy (Zometa) has been shown to harden the outside of bones, therefore reducing the risk of bone fractures, bis. therapy does nothing to treat bone lesions- MM INSIDE the bone.
My overall reply to you is to manage your MM with both conventional (darzalex, pomalyst) as well as non-conventional therapies but I will be more specific about bone health.
As you read in the blog post where I talk about kyphoplasty/vertebroplasty, this therapy can be effective in managing spine lesions. Bone cement injected into the spine effected by MM can kill the MM as well as strengthen the spine.
Another possible therapy is to undergo local radiation. Radiating the lesion can kill the MM at that site. I underwent two rounds of radiation for my bone lesions IN my iliac crest.
- The good new is that the radiation zapped the MM and I felt better within days.
- The bad news is that local radiation for MM, is palliative. Radiation does not kill all of the patient’s MM. The radiation kills the MM at the site of the lesion.
For the record, this palliative therapy bought me months of time during which I researched and found another therapy. But that’s another story.
The overall answer to your question about bone health is to reduce the amount of MM IN your bones. I understand that this is a tall order. The real issue that
I am talking about is embodies in the cure vs. control debate in MM. See the link below.
The challenge that all MM survivors must confront is the idea of balancing the damage done by chemo and the damage done by MM. In your case Frank, you can undergo higher doses of chemo in an effort to kill your MM.
The question is however, will higher doses of chemo, will more toxicity cause other life-threatening health problems? Can you live with “many lesions along my spine, ribs, etc.?” Does the bone involvement that you speak of, cause pain? Does it affect your quality of life?
Your bout of ONJ, osteonecrosis of the jaw is an example of the health problems that chemotherapy can cause. I will link a study below that cites HBOT, Hyperbaric Oxygen Therapy as helping to heal ONJ.
The reply to your question then is, do you want to try to cure your MM or do you want to try to control it? If you want to try to cure your MM, then undergo higher doses of chemo. This increased chemo should reduce the bone lesions IN your bones.
If you want to try to control your MM, undergo reasonable doses of chemo as well as evidence-based, non-toxic, non-conventional therapies. See the MM CC bone health guide below that talks about some of the therapies shown to enhance bone health.
To Learn More about Myeloma and Bone Involvement- click now
Let me know if you have any questions Frank. Good luck.
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Diagnostics- Best Imaging Detecting Bone Involvement
- Cancer Coaching Testimonials- PeopleBeatingCancer
- End Stage for Advanced Multiple Myeloma
Treatment of Myeloma: Cure vs Control
“Although not often openly acknowledged, “cure vs control” is the dominant philosophical difference behind many of the strategies, trials, and debates related to the management of myeloma. Should we treat patients with myeloma with multidrug, multitransplant combinations with the goal of potentially curing a subset of patients, recognizing that the risk of adverse events and effect on quality of life will be substantial? Or should we address myeloma as a chronic incurable condition with the goal of disease control, using the least toxic regimens, emphasizing a balance between efficacy and quality of life, and reserving more aggressive therapy for later?…”
Hyperbaric oxygen therapy for osteonecrosis
“Results
We included two systematic reviews, two RCTs and 13 case series in this health technology assessment. We considered the methodological quality of the systematic reviews as high. The risk of bias we considered unclear in one RCT and high in the other. Because case series are generally considered a poor research design, we did undertake our own quality assessment of this evidence.
One systematic review included three RCTs on effects of HBOT of radiation-related osteonecrosis in the jaw. More patients receiving HBOT achieved complete mucosal coverage at 12- to 18 months’ follow-up, than in control groups (RR 1.30; 95% CI 1.09 – 1.55; 3 studies / 246 participants). We had medium confidence in the effect estimate. The effect estimate of the absence of osteonecrosis after one year was RR 0.60 with 95% CI 0.25 to 1.41 (1 study). Our confidence in the effect rate was very low.
The other systematic review included one RCT that examined the effect of HBOT for drug-related osteoarthritis on healing, compared to standard treatment. The effect estimate was RR 1.56 with 95% CI 0.77 to 3.18 (1 study). Our confidence in the effect estimate was very low.
The two RCTs examined the effect of HBOT for osteonecrosis in the hip joint, but there was only one that reported data from which effect estimates could be calculated…”