
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Treating Multiple Myeloma-Induced Acute Kidney Damage (AKI)-
Treating Multiple Myeloma-Induced Acute Kidney Damage (AKI)-
Both MYRE studies (of MM-induced AKI) remind us that more aggressive therapy is not synonymous with medical benefit.
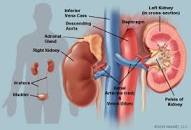
Acute Kidney Injury is both a symptom as well as side effect of Multiple Myeloma patients and survivors. According to research, about half of all MM patients present with some degree of kidney damage at diagnosis.
The challenge however, is how best to heal your kidney function if you can believe the conclusions of studies like the ones linked below.
Or to put this another way, how does the CKD patient also manage his/her multiple myeloma?
Aggressive chemotherapy might damage your kidney function. Not treating your MM may allow it to grow also damaging kidney function more?
Consider low dose Velcade (bortezomib) shown to manage your MM as well as improve your kidney function (see the study linked below).
To Learn More about N-Acetyl Cysteine- click now
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Myeloma Diet- Vegan, Vegetarian, Red Meat?
- Colorectal Cancer- Eat Plenty of Fiber-Reduce Your Risk of Reccurrence
- Multiple Myeloma Chemos That Cause Kidney Damage
Rapid improvement in renal function in patients with multiple myeloma and renal failure treated with bortezomib
“We report here six cases of renal failure secondary to MM treated with bortezomib. All patients had poor performance status of 3-4 on ECOG scale. Five out of six patients showed satisfactory anti-myeloma response to bortezomib. Reversal of renal failure was observed in all six patients. Adverse effects to bortezomib were mild and manageable.
Reversal of renal failure persisted despite incomplete response to MM in two cases, and progression of disease in one patient. It appears that bortezomib may have an effect on the kidneys in reversal of renal failure, other than its anti-myeloma effect. In conclusion, bortezomib appears to be an effective treatment for patients with advanced MM and renal failure irrespective of performance status and age…”
Myeloma-Induced Acute Kidney Injury: Medicine vs Machine
“Nephrologists often consider extracorporeal therapy as a medical advancement…
A good case in point is the MYRE study from 2017 which randomly assigned dialysis-dependent patients with presumed myeloma-induced acute kidney injury (AKI) to high-cutoff vs high-flux dialysis. Patients in the high-cutoff arm experienced more freedom from dialysis after 3 months but the results were not statistically significant. In the subsequent EuLITE trial, high-cutoff dialyzers were associated with more harm (increased infections) than good in patients with myeloma-induced AKI-dialysis.
Trials like these remind us that high-tech isn’t necessarily synonymous with medical progress. That brings us to the 2020 MYRE study, which focuses on medicine rather than high-cutoff dialyzers. Those patients screened for the original MYRE study who did not need hemodialysis were randomly assigned to receive standard care with dexamethasone plus bortezomib vs triple therapy with dexamethasone, bortezomib, and cyclophosphamide. It was hoped that the addition of cyclophosphamide would accelerate time to resolution of AKI…
There was a trend toward quicker resolution of AKI using the triple therapy, but the results were not statistically significant, perhaps owing to the small sample size. Both MYRE studies remind us that more aggressive therapy is not synonymous with medical benefit. Although both MYRE studies were small in size, they teach us a valuable lesson about the disconnect between “intense” treatment and “progress.”
The 2020 MYRE study falls short, in my humble opinion, because it didn’t compare standard therapy against high-flux dialysis for patients with AKI-dialysis…”
Carfilzomib-related acute kidney injury may be prevented by N-acetyl-l-cysteine
“Carfilzomib is a second-generation epoxyketone proteasome inhibitor that is approved for treatment of relapsed and refractory multiple myeloma.
Phase 2 trials have reported that 25% of treated patients have renal adverse effects. Pre-renal/vasoconstriction-related insult from this chemotherapy agent has been documented.
We describe a case of a 78-year-old man with refractory multiple myeloma with acute kidney injury associated with carfilzomib treatment. We show that use of N-acetyl-l-cysteine in our patient partially mitigated the renal injury upon re-challenge.
This case report hypothesizes that acute renal injury from carfilzomib is caused by vasoconstriction of the renal vessels, which may be prevented by N-acetyl-l-cysteine.”
Substituting red meat with alternate dietary proteins may reduce kidney disease risk
“While the consumption of greater quantities of red meat was associated with a higher incidence of chronic kidney disease, researchers from Iran suggest that making substitutions with other sources of dietary protein may reduce the risk…
The researchers contended that meat — described here as “a major source of protein in most diets” — has been demonstrated to have negative health outcomes in contrast to the “favorable effects” seen with plant-based proteins (including whole grains, nuts and legumes)…
After 3-year follow-up, there was a CKD incidence rate of 12.6%, with the researchers finding total red meat intake was associated with a 71% increased risk (odds ratio = 1.73, when comparing those in the highest quartile of consumption to those in the lowest). For processed red meat, they observed a 99% increased CKD risk (OR = 1.99) for participants in the highest compared with those in the lowest quartiles...
Protective effects of three selected standardized medicinal plant extracts used in Sri Lankan traditional medicine in adriamycin induced nephrotoxic Wistar rats
“Results- The plant extracts at the three selected doses significantly attenuated the elevations in serum creatinine, blood urea nitrogen and the loss of urine total protein in a dose related manner in ADR induced nephrotoxic rats (p < 0.001).
The serum concentration of albumin and total protein increased significantly (p < 0.001). Histopathological findings corroborated the biochemical evidence of nephroprotective activity. The aqueous extracts of the three selected medicinal plants exerted a relatively high antioxidant activity in vitro.
Conclusions- Evaluation of the protective effects based on biochemical parameters and histopathology assessment revealed that the aqueous leaf extracts of A. moschatus, A. falcatus and the whole plant extract of B. prionitis possess significant nephroprotective activity against ADR induced acute nephrotoxicity.
The secondary metabolites present in the plant extracts may attribute to the total antioxidant activities of the selected medicinal plant extracts thereby exerting protective effects against nephrotoxicity in Wistar rats.
Highlights
- •Abelmoschus moschatus, Asparagus falcatus, Barleria prionitis are widely used in Sri Lankan traditional medicine for kidney diseases.
- •The aqueous extracts of the selected plants showed protective effects against adriamycin induced acute nephrotoxicity.
- •Barleria prionitis showed the highest nephroprotective activity in vivo.

