Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Immune Checkpoint Inhibitors- Side Effects
Immune Checkpoint Inhibitors- Side Effects

In addition to efficacy data from trials, our findings provide useful information for clinicians for well-balanced discussions with their patients on the risks and benefits of treatment options for advanced cancer…
I am a long-term cancer survivor and cancer coach. I see the studies linked and excerpted below differently than your oncologist. In short, Immune Checkpoint Inhibitors are more dangerous than your oncologist knows.
Lung Cancer
My view of conventional lung cancer therapies is that they offer a poor risk/reward proposition to cancer patients. Especially lung cancer (LC) patients. Conventional therapies, either traditional chemo or immunotherapies, must be supported by evidence-based complementary and integrative therapies.
I don’t mean to suggest that you face lung cancer treatment without conventional therapies at all. My experience is to combine conventional therapies such as immunotherapy with evidence-based, non-toxic, non-conventional therapies.
Cardio-toxicity-
According to the last study linked and excerpted below, ICI are cardiotoxic and can cause a variety of problems to your heart. And keep in mind that that study looked at only five years of evidence.
Pre-Habilitation-
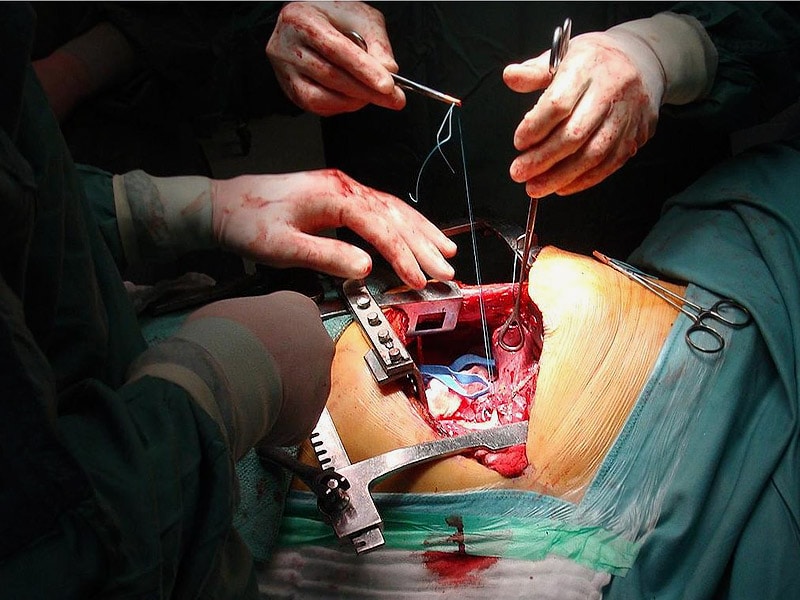
A good example of what I am talking about is pre-habilitating before your surgery, radiation or chemotherapy. And/or enhance your chemo with an integrative therapy such as curcumin.
Or by increasing your fiber intake you may be able to enhance the efficacy of immunotherapy.
Have you been diagnosed with lung cancer? What stage? Please scroll down the page, post a question or comment and I will reply to you ASAP.
thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Early Lung Cancer Therapies Reduce Cancer Deaths Significantly
- Early Lung Cancer, SBRT if Surgery is Not an Option
- The Cure for Lung Cancer May Be in Fish Oil
- Fish Oil Improves Response to Chemo, Improves OS for Lung Cancer Patients
Safety and Tolerability of PD-1/PD-L1 Inhibitors Compared with Chemotherapy in Patients with Advanced Cancer: A Meta-Analysis.
“Background: Compared with chemotherapy, significant improvement in survival outcomes with the programmed death receptor-1 (PD-1) inhibitors nivolumab and pembrolizumab and the programmed death-ligand 1 (PD-L1) inhibitor atezolizumab has been shown in several types of advanced solid tumors. We conducted a systematic review and meta-analysis to compare safety and tolerability between PD-1/PD-L1 inhibitors and chemotherapy…
Results: A total of 3,450 patients from 7 RCTs were included in the meta-analysis: 4 nivolumab, 2 pembrolizumab, and 1 atezolizumab trials. The underlying malignancies included were non-small cell lung cancer (4 trials) and melanoma (3 trials). Compared with chemotherapy, the PD-1/PD-L1 inhibitors had a significantly lower risk of all- and high-grade fatigue, sensory neuropathy, diarrhea and hematologic toxicities, all-grade anorexia, nausea, and constipation, any all- and high-grade AEs, and treatment discontinuation.
There was an increased risk of all-grade rash, pruritus, colitis, aminotransferase elevations, hypothyroidism, and hyperthyroidism, and all- and high-grade pneumonitis with PD1/PD-L1 inhibitors.
Conclusion: PD-1/PD-L1 inhibitors are overall better tolerated than chemotherapy. Our results provide further evidence supporting the favorable risk/benefit ratio for PD-1/PD-L1 inhibitors. The Oncologist 2017;22:470-479 IMPLICATIONS FOR PRACTICE: We conducted a systematic review and meta-analysis to compare summary toxicity endpoints and clinically relevant adverse events between programmed death receptor-1 (PD-1)/programmed death-ligand 1 (PD-L1) inhibitors and chemotherapy. PD1/PD-L1 inhibitors were associated with a lower risk of treatment-related symptoms (fatigue, anorexia, nausea, diarrhea, constipation, and sensory neuropathy) but a higher risk of immune-related adverse events (AEs). Summary toxicity endpoints favor PD1/PD-L1 inhibitors (any all- and high-grade AEs and treatment discontinuation). PD1/PD-L1 inhibitors are overall better tolerated than chemotherapy. In addition to efficacy data from trials, our findings provide useful information for clinicians for well-balanced discussions with their patients on the risks and benefits of treatment options for advanced cancer.
Flu Vaccine in Lung Cancer Patients Could Increase Immunotherapy Toxicities
“Seasonal influenza vaccination resulted in increased risk of immune-related adverse events (AEs) in lung cancer patients treated with PD-1/PD-L1 checkpoint inhibitors in a small study. However, the risks of the flu itself may still outweigh the risks associated with vaccination…
“Although routine influenza vaccination has long been recommended for cancer patients, there are concerns that it might trigger an exaggerated immune response in this subgroup receiving checkpoint inhibitors…”
The vaccine was effective in all patients, with no reported cases of influenza. There was an unusually high frequency of immune-related AEs, however, occurring in 52.2% of patients; six patients (26.1%) had a grade 3 or 4 immune-related AE. The most common such AEs were skin rashes and arthritis (13% each), colitis and encephalitis (8.7% each), and hypothyroidism, pneumonitis, and neuropathy (4.3% each)…
“The frequency is significantly higher than the rate of immune-related AEs in unvaccinated patients treated with PD-1/PD-L1 inhibitors,” Rothschild said. At his center, the expected rate of such AEs would be about 25.5%; rates between 30% and 35% have been reported in the literature. “Our hypothesis is that the vaccine results in an overwhelming activation of the immune system in this population.” He added, though, that “there is a particular concern for severe complication of an influenza infection including pneumonia and respiratory failure for patients with lung cancer under immunotherapy….”
Immune checkpoint inhibitor therapy linked to higher incidence of cardiovascular events
“Immune checkpoint inhibitor therapy appeared associated with an increased risk for major adverse cardiovascular events among patients with cancer and a prior history of cardiovascular disease, according to results of a retrospective study…
“Another limitation of the currently available data is that randomized clinical trials of ICIs focus on survival, response and disease control, usually [during] short follow-up periods…”
Researchers reported a 10.3% incidence of major cardiovascular events, with a median time to event of 5 months…
“Concomitant cardiovascular disease is often an exclusion criterion in clinical trials. This might be one of the reasons why this type of toxicity is underreported in phase 3 trials. In addition, toxicity is often not part of the follow-up when treatment within the context of the study is ceased. Cohort studies like ours can compensate for these shortcomings…”