
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Cervical Cancer- AHCC?
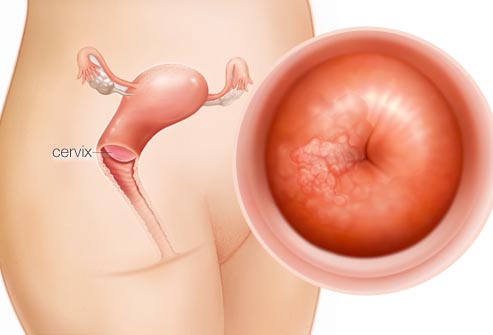
Cervical Cancer- AHCC?
Hi David- My question is about AHCC suprementation. I was diagnosed with Cervical Cancer in April 2022. I took Radiation and Chemo Treatments for most of September and 3 Weeks in October. I was declared free of Cancer on December 14, 2022, just 6 days ago.
Today I was reading Dr. Pescatori’s book about Cancer and he suggested AHCC, as one of the supplements. While looking for more info about AHCC, I found your site.
My question is if HPV causes Cervical Cancer, then do I have HPV without knowing it? and do I need to take AHCC to eradicate it?
Dear Cervical Cancer Survivor-
I am happy to read that you have reached remission aka cancer free status. Two issues to consider.
- Decreasing your risks of long-term and late stage side effects
- Decreasing your risks of relapse
I am discussing your risks of long-term and late stage side effects for several reasons. I am assuming that your radiation treatment involved your pelvic region. Research linked and excerpted below explains possible side effects of radiation better than I can.
Long story short, please consider evidence-based but non-conventional therapies shown to heal radiation damage. I take probiotics as well as several anti-inflammatory nutritional supplements myself. I underwent radiation to my lower back myself. Radiation is double-edged sword.
I will excerpt information that cites hyperbaric oxygen therapy (HBOT) as well an nutritional supplementation that have been shown to health radiation fibrosis. I also encourage you to talk to your oncologist about possible side effects of pelvic radiation.
If your oncologist prescribes HBOT therapy then your health insurance should cover it. Also, please don’t wait before trying to heal possible radiation damage.
As for decreasing your risk of relapse. This is where AHCC supplementation comes in to your situation. In order to determine your HPV status, you should talk to your oncologist and be tested. Yes, HPV increases your risk of cervical cancer. Yes, according to the research below, AHCC supplementation can clear HPV. While I cannot cite research, I think that clearing your body of HPV can reduce your risk of a relapse.
Lastly, I have to plug the benefit of evidence-based, non-conventional therapies shown to reduce the risk of cervical cancer aka reduce your risk of relapse.
- Curcumin has been shown to fight both cervical cancer as well as HPV.
- Omega-3 fatty acids have been shown to help cervical cancer patients as well.
- Resveratrol has also been shown to inhibit the progression of cervical cancer.
In short, the therapy you have already undergo is great to have gotten rid of your cervical cancer but, in my experience, preventing side effects and possible relapse is central to cancer management as well.
Feel free to ask any and all questions.
Hang in there,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Research as shown me that cervical cancer has a lot in common with my blood cancer, multiple myeloma.
- HPV Variable Risk Factor in Cervical Cancer
- Ultrasound-Curcumin treatment kills cervical cancer
- Primary Cervical Cancer-Secondary Cancer
- Anti-angiogenesis Extends Cervical Cancer Survival
- AHCC Cured My Human PapillomaVirus – Cervical Cancer?
Pelvic radiation therapy: Between delight and disaster
“Pelvic radiation disease (PRD) can result from ionising radiation-induced damage to surrounding non-cancerous tissues resulting in disruption of normal physiological functions and symptoms such as diarrhoea, tenesmus, incontinence and rectal bleeding. The burden of PRD-related symptoms, which impact on a patient’s quality of life, has been under appreciated and sub-optimally managed. This article serves to promote awareness of PRD and the vast potential there is to improve current service provision and research activities…
Radiotherapy to organs of the pelvis renders the bowel at risk of radiation induced injury, a condition recently coined pelvic radiation disease (PRD)[4,5]. This term encapsulates conditions including
- radiation enteritis,
- radiation proctitis and
- radiation cystitis[6]
which inaccurately depict the condition as an ongoing inflammatory process. In fact, after the initial three months the inflammation is largely replaced by progressive ischaemia and fibrosis of tissues. This radiation induced damage to healthy tissue around the tumour could be a major limiting factor to curative treatment of localised cancer as treatment regimes may be interrupted…
MANAGEMENT
How to manage patients with PRD is a contentious subject. It was largely believed to be untreatable until a better understanding of the aetiology and pathogenesis paved the way for a paradigm shift in treatment. Medicines, dietary modifications and supportive measures are some of the components of current guidelines. In the majority of cases the cornerstone of management after prevention is symptom control. Symptoms can originate from a variety of affected sites therefore a crucial step in PRD management is the understanding that urological, gastrointestinal, gynaecological, dermatological, lymphatic, nervous, vascular structures and sexual organs can be involved…
Hyperbaric oxygen therapy
Hyperbaric oxygen (HBO) therapy has been utilised to treat chronic PRD for several decades[54] but with insufficient evidence of its exact mechanism of action or to support its use in clinical practice. More recently HBO has been found to decrease tissue hypoxia by inducing angiogenesis in bowel affected by the ischaemic and fibrotic changes associated with chronic PRD changes[55]. Clarke et al[56] (2008) conducted the first randomised control trial and provided support for its use in refractory PRD.
Specifically, HBO induced healing responses and was associated with an absolute risk reduction of 32%. Furthermore, bowel specific quality of life was improved. HBO treatment does require a significant time commitment, logistical hurdles and is expensive to fund. A complete regime consists of eight weeks of daily treatment in a specialist unit that typically have vast catchment areas[5].
AHCC® Supplementation to Support Immune Function to Clear Persistent Human Papillomavirus Infections
“Results
Fifty women with high-risk HPV were enrolled, and 41 completed the study. Fourteen (63.6%) of the 22 patients in the AHCC supplementation arm were HPV RNA/HPV DNA negative after 6 months, with 64.3% (9/14) achieving a durable response defined as being HPV RNA/HPV DNA negative 6 months off supplementation.
On the placebo arm, two (10.5%) of 19 patients were HPV negative at 12 months. In the twelve placebo arm patients who elected to continue on the unblinded study, 50% (n = 6) were HPV RNA/HPV DNA negative after 6 months of AHCC supplementation. At the time of completion of the study, there were a total of 34 patients (22 blinded and 12 unblinded) who had received AHCC supplementation with an overall response rate of 58.8% that cleared HPV persistent infections.
At the time of enrollment, the mean IFN-β level was 60.5 ± 37.6 pg/ml in women with confirmed persistent HPV infections. Suppression of IFN-β to less than 20 pg/ml correlated with an increase in T lymphocytes and IFN-γ and durable clearance of HPV infections in women who received AHCC supplementation…


